
DEFINITION:
is a vector-borne infectious disease caused by protozoan parasites. It is widespread in tropical and subtropical regions, including parts of the Americas, Asia, and Africa. Each year, there are approximately 515 million cases of malaria, killing between one and three million people, the majority of whom are young children in Sub-Saharan Africa.
Is a serious, infectious disease spread by certain mosquitoes. It is most common in tropical climates. It is characterized by recurrent symptoms of chills, fever, and an enlarged spleen. The disease can be treated with medication, but it often recurs. Malaria is endemic (occurs frequently in a particular locality) in many third world countries. Isolated, small outbreaks sometimes occur within the boundaries of the United States.
SYMPTOMS
When symptoms appear
The time from the initial malaria infection until symptoms appear (incubation period) generally ranges from:1
- 9 to 14 days for Plasmodium (P.) falciparum.
- 12 to 18 days for P. vivax and P. ovale.
- 18 to 40 days for P. malariae.
Symptoms can appear in 7 days. Occasionally, the time between exposure and signs of illness may be as long as 8 to 10 months with P. vivax and P. ovale.
The incubation period may be longer if you are taking medicine to prevent infection (chemoprophylaxis) or because you have some immunity due to previous infections.
Variation in symptoms
In regions where malaria is present, people may have the disease but—due to immunity or semi-immunity—they have few or no symptoms.2 The severity of malaria symptoms can also vary depending on your immunity, your general health, and whether you still have your spleen.
Common symptoms of malaria
In the early stages, malaria symptoms are sometimes similar to those of many other infections caused by bacteria, viruses, or parasites. Symptoms may include:
- Fever.
- Chills.
- Headache.
- Sweats.
- Fatigue.
- Nausea and vomiting.
Symptoms may appear in cycles and may come and go at different intensities and for different lengths of time. However, especially at the beginning of the illness, the symptoms may not follow this typical pattern.
The cyclic pattern of malaria symptoms is due to the life cycle of malaria parasites as they develop, reproduce, and are released from the red blood cells and liver cells in the human body. This cycle of symptoms is also one of the major indicators that you are infected with malaria.
Other common symptoms of malaria
Other common symptoms of malaria include:
- Dry (nonproductive) cough.
- Muscle and/or back pain.
- Enlarged spleen.
Rarely, malaria can lead to impaired function of the brain or spinal cord, seizures, or loss of consciousness.
Infection with the P. falciparum parasite is usually more serious and may become life-threatening.
There are other conditions with symptoms similar to a malarial infection. It is important that you see your doctor to discover the cause of your symptoms.
TREATMENT
Treatment Overview
Medication can prevent malaria and is necessary to treat the disease. Several factors influence the choice of medication, including:
- Whether the medicine is being used to prevent or to treat malaria.
- Your condition (such as your age or whether you are pregnant).
- How sick you are from malaria.
- Geographic location where you were exposed to malaria.
- Whether the malaria parasite may be resistant to certain medications.
- Your ability to take the preferred medicine without side effects or complications.
- Whether you are able to take the medication as a pill.
Malaria is rare in the United States, but it is widespread in other parts of the world. Find out about the risk for malaria before you travel internationally. The most accurate information about malaria risk and medication resistance in specific countries is from the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
If you have malaria, medication choice is based on:
- The specific parasite causing the infection.
- The severity of the infection.
- Your condition (such as age, pregnancy, allergies, or health problems).
- Medication resistance of the parasite found in the geographic area where you were infected.
If you have been in an area where malaria occurs, were exposed to mosquitoes, and develop flu-like symptoms, but tests do not show the malaria parasite in your blood, the tests should be repeated 3 or 4 times to confirm that you do not have a malaria infection. During medication treatment, tests are repeated to follow the course of the infection and to check whether the number of parasites is decreasing.
Your age and health condition are important factors in selecting a medication to prevent or treat malaria. Pregnant women, children, people who are very old, people who have other health problems, and those who did not use medication therapy to prevent malaria infection require special consideration.
Treatment
Active malaria infection with P. falciparum is a medical emergency requiring hospitalization. Infection with P. vivax, P. ovale or P. malariae can often be treated on an outpatient basis. Treatment of malaria involves supportive measures as well as specific antimalarial drugs. When properly treated, someone with malaria can expect a complete recovery.[73]
Antimalarial drugs
There are several families of drugs used to treat malaria.
- Artemether-lumefantrine (Therapy only, commercial names Coartem and Riamet)
- Artesunate-amodiaquine (Therapy only)
- Artesunate-mefloquine (Therapy only)
- Artesunate-Sulfadoxine/pyrimethamine (Therapy only)
- Atovaquone-proguanil, trade name Malarone (Therapy and prophylaxis)
- Quinine (Therapy only)
- Chloroquine (Therapy and prophylaxis; usefulness now reduced due to resistance)
- Cotrifazid (Therapy and prophylaxis)
- Doxycycline (Therapy and prophylaxis)
- Mefloquine, trade name Lariam (Therapy and prophylaxis)
- Primaquine (Therapy in P. vivax and P. ovale only; not for prophylaxis)
- Proguanil (Prophylaxis only)
- Sulfadoxine-pyrimethamine (Therapy; prophylaxis for semi-immune pregnant women in endemic countries as "Intermittent Preventive Treatment" - IPT)
- Hydroxychloroquine, trade name Plaquenil (Therapy and prophylaxis)
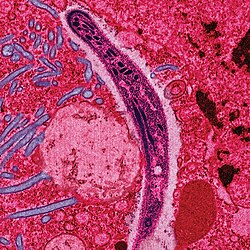
CAUSATIVE AGENT
WUCHERERIA BANCROFTI MICROFILARIAPlasmodium sporozoites initiate malaria infection in the human host. Their journey, from the midgut wall of the mosquito to the human liver is the focus of our research. Sporozoites develop in oocysts on the midgut wall of infected mosquitoes, are released into the hemocoel and invade salivary glands where they wait to be injected into a vertebrate host during the mosquito’s bloodmeal.
We have shown that the major surface protein of sporozoites binds preferentially to mosquito salivary glands compared to other organs in the hemocoel. We are currently characterizing the salivary gland molecule(s) which are responsible for this recognition.

MODE OF TRANSMISSION
The female anopheles mosquito is the vector for human malaria. Some 60 species of this mosquito have been identified as vectors for malaria, and their distribution varies from country to country. When a mosquito bites an infected individual, it sucks the gametocytes, the sexual forms of the parasite, along with blood. These gametocytes continue the sexual phase of the cycle and the sporozoites fill the salivary glands of the infested mosquito. When this female mosquito bites the man for a blood meal, which it needs to nourish its eggs, it inoculates the sporozoites into human blood stream, thus spreading the infection.
The female anopheles mosquito bites man between 5 PM and 7 AM, with maximum intensity at midnight.
1. Blood transfusion (Transfusion malaria): This is fairly common in endemic areas.
Following an attack of malaria, the donor may remain infective for years (1-3 years in P. falciparum, 3-4 years in P. vivax, and 15-50 years in P. malariae.)
Most infections occur in cases of transfusion of blood stored for less than 5 days and it is rare in transfusions of blood stored for more than 2 weeks. Frozen plasma is not known to transmit malaria.
The clinical features of transfusion malaria occur earlier and any patient who has received a transfusion three months prior to the febrile illness should be suspected to have malaria.
Donor blood can be tested with indirect fluorescent antibody test or ELISA, and direct examination of the blood for the parasite may not be helpful.
In endemic areas, it is safe to administer full course of chloroquine to all recipients of blood transfusion.
In transfusion malaria, pre-erythrocytic schizogony does not occur and hence relapses due to dormant hepatic forms also does not occur. Therefore, treatment with primaquine for 5 (or14) days is not indicated.
2. Mother to the growing fetus (Congenital malaria): Intrauterine transmission of infection from mother to child is well documented. Placenta becomes heavily infested with the parasites. Congenital malaria is more common in first pregnancy, among non - immune populations.
3. Needle stick injury: Accidental transmission can occur among drug addicts who share syringes and needles. (Therapeutic inoculation of malarial parasites, so as to induce fever, was a mode of treatment for neurosyphilis!)
PHOTOS
 |  |
|---|
 REFERENCES:
REFERENCES:http://www.med.nyu.edu/parasitology/faculty/psinnis.html
http://en.wikipedia.org/wiki/File:Anopheles_albimanus_mosquito.jpg
http://www.malariasite.com/malaria/Transmission.htm

No comments:
Post a Comment